-
10 Mar, 2017
-
Author/blogger Reggie Simpson
Parliament debates workplace dress codes
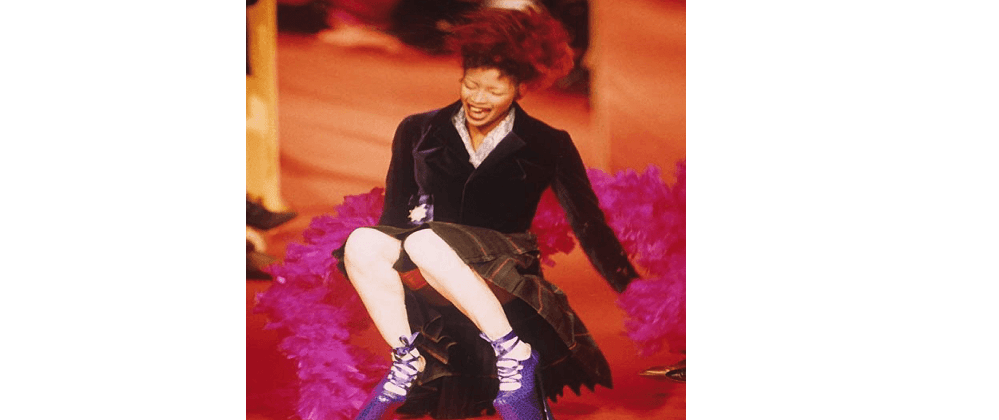
Remember when Naomi Campbell tripped and fell on the catwalk wearing super high platform shoes during a Vivienne Westwood show in 1993? She laughed it off; we guffawed. Here was one of the top supermodels dubbed the ‘Trinity’ purported to ‘not wake up for less than $10,000 a day’.
I suppose Campbell’s ‘fall from grace’ was an occupational hazard.
Speed forward to 2017. The average woman can hardly afford to lounge in bed, and she most likely (and sensibly) will not totter around in platform shoes in the workplace. However, high heels and other compulsory dress code attire for women have become symbols of workplace sexism and discrimination.
In a week that celebrated International Women’s Day (‘Be Bold for Change’), Parliament convened a meeting on 6 March to consider an e-petition submitted by Nicola Thorp focused on high heels and workplace dress codes. The petition had 152,420 signatures.
In December 2015, Ms Thorp was sent by Portico for a job as a temporary receptionist at the headquarters of PriceWaterhouseCoopers in London. When she arrived, Ms Thorp was told that the smart black shoes she was wearing were unacceptable because they were flat; at the time, Portico’s dress code specified a heel height of between two and four inches—for women, not men. She was offered the opportunity to go out and buy a pair of high heels. When she refused, she was sent home without pay.
Speaking on behalf of the petition, Helen Jones (Warrington North, Lab) MP said:
‘There was never a suggestion that Ms Thorp was not smartly dressed … Secondly, it was clear that wearing high heels was a requirement that impacted far more on women than on men. In fact, most of Portico’s dress code at the time was about how women should look. Not only were women to wear high heels but they were compelled to wear make-up’.
When the issue was first raised with the parliamentary Petitions Committee and the Women and Equalities Committee this past January, there was shock and disbelief that such workplace attitudes and practices still exist.
Make-up and dress aside, we at Betafeet Podiatry and within the wider foot care profession take particularly interest in High Heel Gate (or is that High Hell Gate?).
According to the Hon MP Jones:
‘There are people who think that we should not have investigated this at all—in fact, they think it is a bit of a joke. Yes, it is true that women sometimes wear high heels, but there is plenty of evidence about the damage from wearing heels long term; that is well known and has been for some time. We received written evidence from the College of Podiatry and individual podiatrists on our web forum setting out just what that damage is. Wearing high heels long term alters balance, reduces flexion in the ankle and weakens calf muscles. Over time, that can make women much more prone to a number of problems, including stress fractures, Morton’s neuroma, ankle sprains and bunions, and it causes a reduction in balance that lasts into old age, putting people more at risk of falls’.
See Betafeet Podiatry’s previous blog on the effects of wearing high heels:
https://www.betafeetpodiatry.co.uk/the-risks-of-high-heels-and-how-to-avoid-them
From a corporate risk assessment standpoint, companies should review their dress code policy, not least for health and safety reasons, but also reputational risk and/or litigation consequences. To its credit, Portico has since changed its dress code policy.
Watch this space for further steps, hopefully in the right direction.
Note: Men, please forgive me for not commenting on any of your own possible workplace dress code issues. That is for another parliamentary debate.