-
21 Sep, 2016
By Matthew Collison
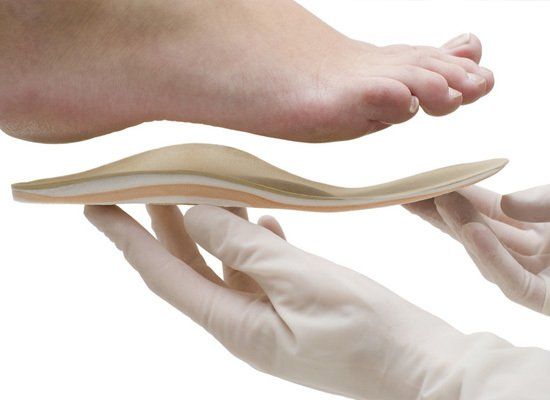
Foot orthoses are often prescribed for foot and lower limb pain. The main way that orthoses work is by altering the way your foot interacts with the ground when you walk or run. The aim of an orthosis should be to reduce pathological forces acting on the foot, whether that be to pain in a tissue such as the plantar fascia (heel pain) or to prevent skin breakdown in patients with diabetic neuropathy (sensory loss related to diabetes).
The way forces act on an object (such as the foot) are called kinetics, and the movement and angle of these forces is called kinematics. Often, orthoses are sold to ‘improve alignment’ or to ‘straighten’ feet and joints with the hope of reducing pain; however often it is not necessary or achievable or desirable to modify kinematics with an orthosis. The focus of treatment should be on reducing the kinetics or forces within tissues to reduce pain, rather than purely on alignment.
Different materials and shapes of orthoses can have different effects on tissues, some materials such as low density foams can provide cushioning, whereas other materials like carbon fibre or polypropylene provide more support. Even the top covers can affect the way the orthosis works.
Foot orthoses have been shown to be useful in the management of foot pain in chronic conditions such as rheumatoid arthritis and juvenile idiopathic arthritis as well as specific lower limb pathologies such as plantar fasciitis (heel pain), medial tibial stress syndrome (shin splints), pes cavus (high arches), to name a few.
What kinds of orthoses does Betafeet Podiatry offer?
We offer a wide range of orthoses, ranging from simple wedges, pads or props added to your existing footwear, to prefabricated devices and fully custom devices made from moulds of your feet. Following a biomechanical assessment, your specialist podiatrist at our Tring or Hemel clinic will advise you on what is most appropriate for your needs, and will often offer you a choice of appropriate interventions based on your condition. The key is finding the right tool for the job. You may also find that you need different devices for different footwear or activities. For example, a runner, cyclist or hiker taking on the roads in and around Ashridge or the Tring reservoirs will likely need different devices for his or her running shoes and for their work shoes. Betafeet Podiatry also sees clients who are on their feet most of the day such as those who work in restaurants in Tring and Hemel, and surrounding areas, as well as hairdressers, builders and others.
Orthoses will almost always be prescribed alongside other advice and interventions such as activity modification, stretching and strengthening exercises, self-massage advice and footwear advice.
Stayed tuned for further orthoses blogs.