24 Oct, 2016
Author/blogger Reggie Simpson
Introducing an Exciting New Treatment at Betafeet Podiatry
What is Swift©?
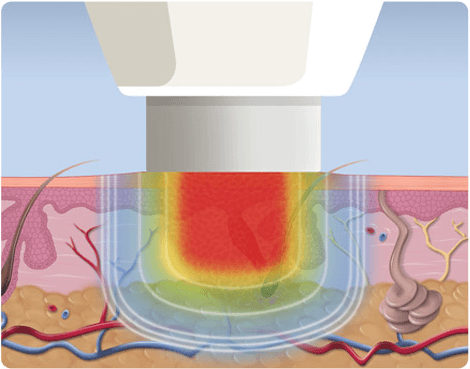
Swift is a new technology, developed in the UK, which has been licensed for the general treatment of verrucae or warts in Podiatry. Swift uses microwave energy that is delivered through a special probe applied to the skin to treat the affected area. Betafeet will be one of only a few clinics in the UK to offer this treatment.
How does it work?
Microwaves work by applying the probe from which heat under the probe is applied to the verruca. The probe is about 7mm in diameter. Usually the largest or most painful verruca is treated first, but multiple ones may be treated at the same time.
Am I eligible for Swift treatment?
Your podiatrist will make a full assessment and discuss whether Swift treatment can help you and advise whether you are eligible. If you have tried various verruca treatments to no effect, then Swift microwave energy at Betafeet Podiatry might be for you. However, precautions include:
- The presence of metal in your foot or ankle
- If you wear a pacemaker
- If you have poor or limited healing capacity because of neuropathy or peripheral circulation
- Patients who are immuno suppressed
- Pregnancy – the effect of verruca/e treatment is reduced during this time
Does it hurt?
Like many treatments for verrucae, some minor discomfort may be experienced. Before treatment your podiatrist will reduce the verruca/e with a blade so the treatment site is level to receive the probe, which is applied for 5 seconds. Pain levels vary from person to person but most people undergoing Swift liken it to a pain similar to an injection or a scratch, lasting 2 - 3 seconds then quickly subsiding. Paracetamol can help if required.
How many treatments will I need?
This is dependent on how you respond to treatment. In some cases, you may need more than one treatment (these can be from 14 days to over a month apart depending on the response). Microwave energy treatment is normally conducted over 3-4 treatments. Larger or numerous verrucae may need more. The verruca/e will go dark, but you won’t see much shrinkage or debulking at first. Your Podiatrist will discuss this all with you.
What can I do after treatment?
In some cases the treated area may feel sore but will not prevent you from undertaking normal daily activities.
I am interested - what do I do next?
If you would like to discuss this further, please call Betafeet Podiatry on 01442 822990 (Tring) or 01442 249080 (Hemel) for an assessment appointment. The podiatrist will be able to assess your feet and advise you if you are suitable for treatment as well as suggesting the treatment plan which is best for you. The podiatrist can also give you an idea on the likelihood of success. This will also give you any opportunities to ask questions about the treatment.
Of course, you are under no obligation to have the treatment and your podiatrist can advise you on other treatments if Swift is not for you. Bear in mind that no verruca treatment can be guaranteed 100% successful and Swift is no exception.